Of waste diverted from landfills at Mahindra Blues Festival 2024
What we do
We bring together diverse, future-facing industries and communities to co-create a positive world, where one enables the other to Rise.
提前知道:幸运澳五历史开奖官方、澳洲幸运5奖历史正规开奖结果,最准开奖计划
The zero-waste approach at Mahindra festivals exemplifies our commitment to sustainability.
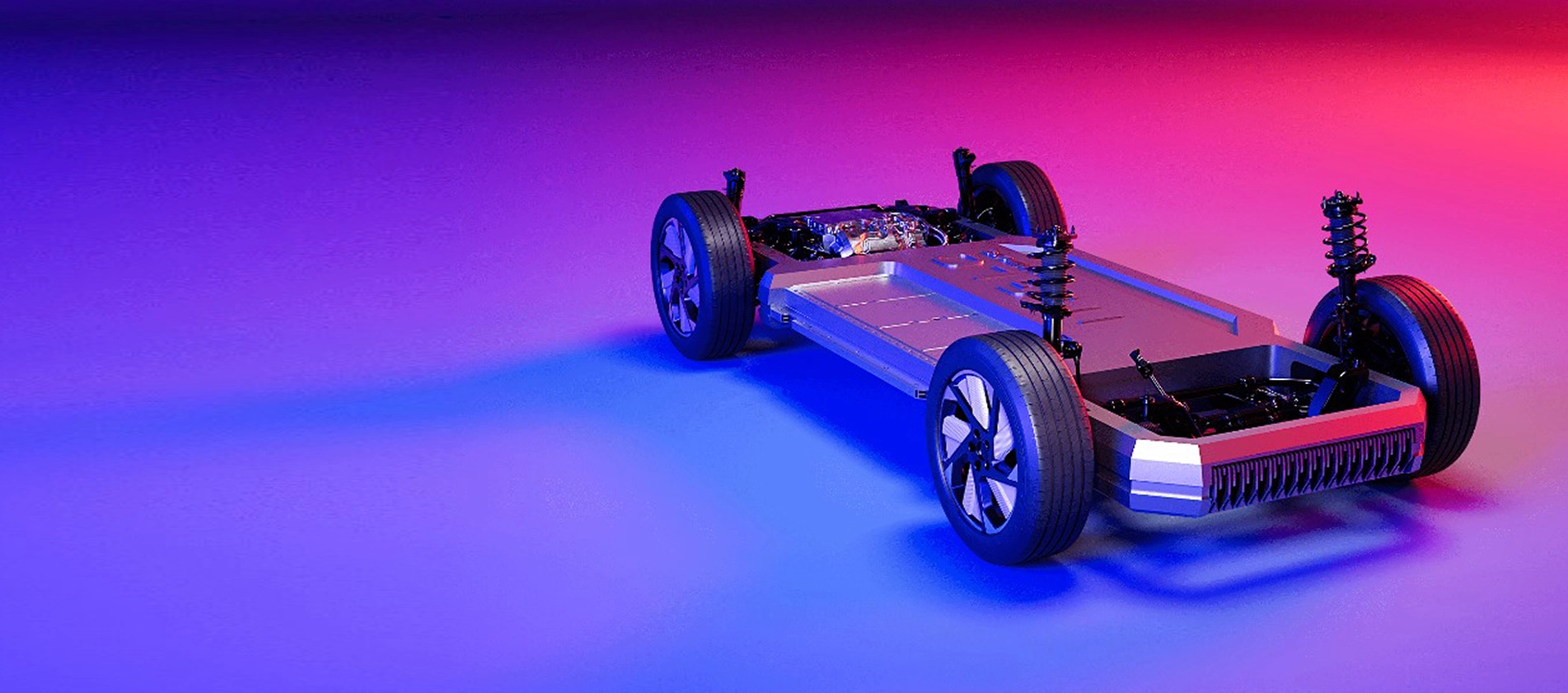
Rise to be future-ready
Using technology to elevate customer experiences.
168澳洲幸运5开奖结果历史查询-手机版开奖最新版
Mahindra Group's Financial Highlights
Work with us
Faqs
-
How many companies are part of the Mahindra Group?
Mahindra & Mahindra is the flagship company of the Mahindra Group which has over 100+ subsidiaries. Of these, 8 are publicly listed. The Group is present in over 20+ industries across Auto, Farm and Services. Our Auto sector includes SUVs, LCVs, electric 3-wheelers, trucks & buses and motorcycles. We are world's largest tractor company by volume. In services we have Mahindra Finance and Tech Mahindra. We are also present in hospitality, real estate, renewables, logistics, steel manufacturing, auto recycling, defence and aerospace. Full list of Mahindra Group of Companies is available in the annual report on our website - https://www.mahindra.com/annual-report-FY2023/index.html
-
Is Mahindra a public or private company?
The Mahindra Group has 8 public companies and many private companies under its umbrella. The parent company, Mahindra & Mahindra Limited is publicly listed. Other listed companies are Tech Mahindra Limited, Mahindra & Mahindra Financial Services Limited, Mahindra Holidays and Resorts India Limited, Mahindra Lifespace Developers Limited, Mahindra Logistics Limited, Mahindra EPC Irrigation Limited, and Swaraj Engines Limited. The group has consistently created value for its shareholders since inception.
-
What is the work culture like at Mahindra?
At Mahindra, performance is deep rooted in purpose. Employees are committed to uplifting communities, guided by the core values and behaviours of being ethical, collaborative, agile, and bold. Mahindra group fosters an inclusive work culture, free from biases, promoting diversity, inclusion, and equitable growth opportunities across all levels. Our path-breaking five-year maternity policy provides support for mental and physical wellbeing of new mothers. Check out our website to know more about various career growth programs and DEI initiatives at Mahindra https://www.mahindra.com/career
-
Where is the headquarters of Mahindra located?
Mahindra Group is a global organization, present in over 100+ countries. The corporate head office of the Mahindra Group is located in Mumbai at Mahindra Towers, Dr. G.M.Bhosale Marg, P.K.Kurne Chowk, Worli - 400018. Head office address of Mahindra & Mahindra and other group companies an be found on our website. You may also contact us via email mentioned here https://www.mahindra.com/contact-us.